
Climate Change: The biggest threat facing humanity
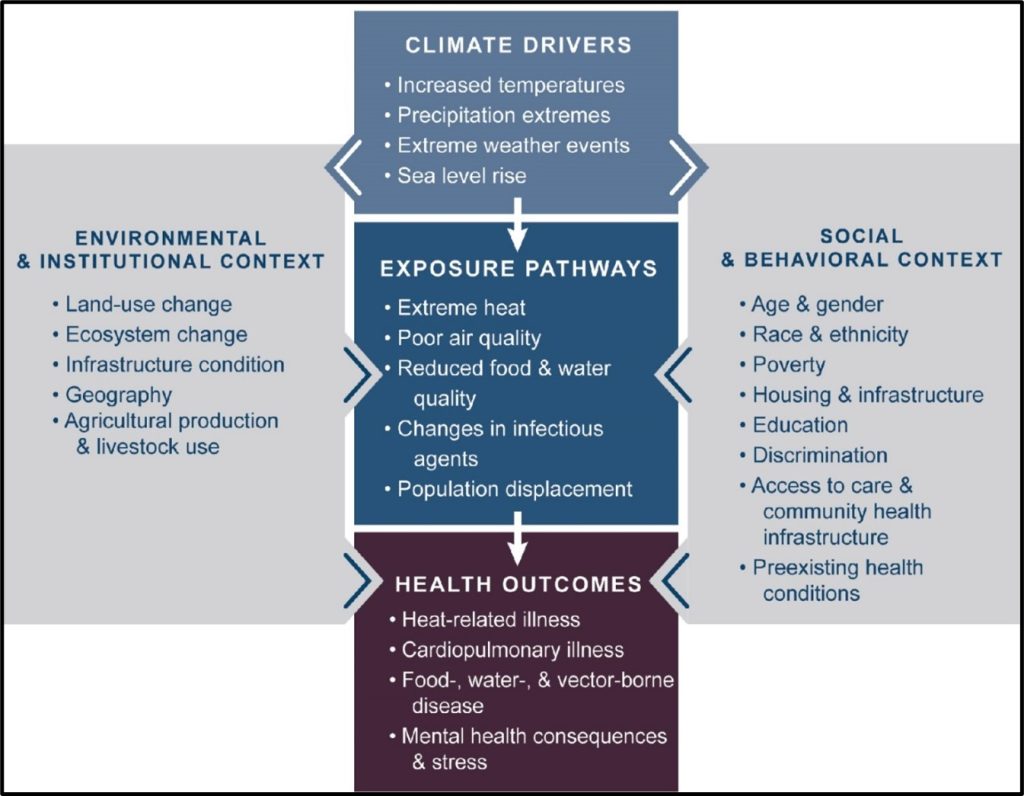
Human beings are exposed to health risks (disease) depending upon inherent factors (e.g., age, gender, and race), lifestyle or behavioural factors (e.g., excess weight, physical inactivity, or tobacco use), and environmental factors (e.g., exposure to air pollution). The environment is a significant determinant of our health and well-being. And we depend on the environment for critical elements, such as clean air, safe drinking water, secure shelter, and sufficient food to sustain life. But climate change affects social and environmental determinants, causing health problems like respiratory diseases, heart disease, and cancer. Environmental health is, thus, a crucial part of any comprehensive public health system.
As per the IPCC report, global heating of even 1.5°C is not safe for humans; however, every additional tenth of a degree of warming will seriously affect people’s lives and health. People in low-income groups are more vulnerable to living in polluted areas and have unsafe drinking water. Pregnant women and children are at a higher risk of pollution-related health problems. The main barriers to healthcare for vulnerable populations are numerous, like poor economy and limited economic resources, high unemployment rates and low education, high rates of uninsurance and underinsurance; and cultural differences that may pose challenges and prevent patients from accessing care.
Climate-Sensitive Health Risks
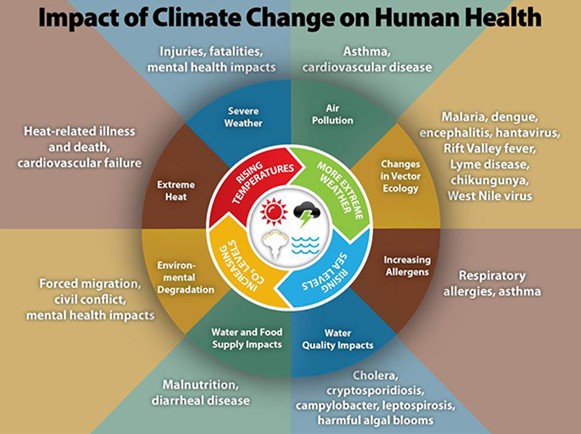
Over the past five years, more than a quarter (27%) of the world’s population has experienced severe weather-based disasters. In response to increased natural and human-made hazards, the exposure of groups or individuals to stress due to the impacts of climate and weather extremes has risen considerably. A warmer world has already led to the increased severity and frequency of many climate hazards – including heatwaves, wildfires, droughts, heavy downpours and floods, melting glaciers, severe coastal storms, coastal inundation due to sea level rise, and expanding ranges of tropical diseases and pests. Millions of people face greater risks to their health because of climate change, including increased risk of air pollution and extreme weather events, among other challenges. Climate change encircles rising average temperatures, shifting wildlife populations and habitats, and other impacts that could further wreak havoc on people’s livelihoods and communities. All these changes are emerging as humans continue adding heat-trapping greenhouse gases to the atmosphere.
- An increase in the number of premature heat-related deaths in the summer is likely as climate change worsens and dangerous weather events become more frequent.
- Increasing concentrations of atmospheric carbon dioxide and altered precipitation patterns are expected to contribute to rising levels of some airborne allergens and an increase in asthma episodes and other allergic illnesses.
Between 2030 and 2050, it is anticipated that climate change will cause approximately 250000 additional deaths per year, only from malnutrition, malaria, diarrhea, and heat stress (Figure 1).
Impact on the Health Sector
The medical field faces four prominent challenges currently: service integration, service quality, internet-connected medical device security, and publicly sustainable pharmaceutical pricing. A resilient society or healthy community fosters good emotional and mental health for all and, further, requires minimization of cascading and compound health hazards due to climate change (Figure 2). As global warming hampers access to health services and the quality of services, it can lead to significant financial losses for healthcare delivery systems. Climate change also exacerbates existing inequities in health and health care. It calls for strengthening health infrastructure and additional health professionals for:
- Assessing probability – gain exclusive data on rising climate-related risks to framing strategies for treatment and cure we envisage for resilience.
- Identifying vulnerability – understand key indicators to overcome common pitfalls of resilience planning.
- Understanding important aspects of resilience – exploit and maximize the resilience strengths in the countries/regions and seasons while taking action to address the gaps and missing links.
The Future Ahead
Global climate change has a particularly detrimental effect on health in vulnerable countries, where health systems are often incapable of managing existing health hazards and adapting to additional risks from climate change.
As part of the solution, efficient health management systems should address the barriers and create a community-wide population health learning system considering the vulnerable population and those needing special care and support because of age, disability, abuse risk, or neglect decisions.
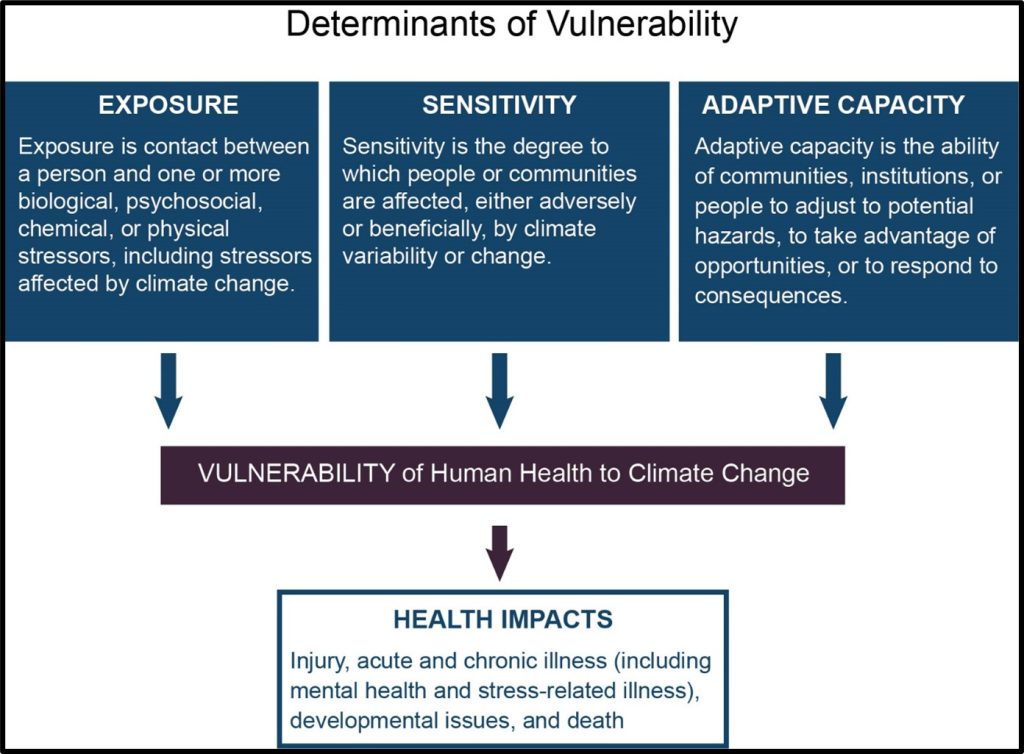
It is highly recommended to create a comprehensive data bank on impending health risks to humans due to site-specific thermal stress, exposure to excessive humid/dry environment (floods and droughts) and related cardiovascular, kidney, and respiratory disorders, airborne/waterborne / vector diseases (weather/climate pertaining), exotic mosquito-borne diseases, e.g., malaria and dengue fever, food insecurity and malnutrition, mental health and stress-related disorders, allergens and pollen, asthma, and respiratory tract infections in a province, community or region in a pilot study and use expert judgment to identify the vulnerability in selective age/gender groups (vulnerable groups could include those with low income, anxiety, and distress induced migrated communities and peoples, children, pregnant women, post-traumaticolder adults with pre-existing health conditions, and persons with disabilities).
The key objective here would be to identify the severity of climate impacts, health outcomes, and the populations and locations vulnerable to health impacts (Figure 3) in India, with the world’s second-largest population. The data bank would also facilitate us in developing a digital tool for health professionals to determine the effects of climate change on local health and the impact on health systems and design interventions for the health impacts of the most significant concern. The vulnerability indices developed with this digital tool would be interrelated with location-specific or hospital-specific availability of a select category of medical professionals/devices and location-specific available pharmaceutical brands/prices.
We must establish a possible linkage among the relevant parameters/indices and create a spatial-temporal decision matrix to plan for implementation and evaluate the effectiveness of the interventions within the sophisticated mapping of risk factors and social vulnerabilities for enhanced sustainability and resilient measures in healthcare. In addition, the identification of some barriers or challenges that might make this process difficult shall be undertaken.
The Covid-19 pandemic has demonstrated the significance of healthcare in ‘today’s world. Therefore, one of the critical aspects of life must be qualitative to disseminate preventive and therapeutic care while embracing modern and old-age healthcare techniques.
The Healthcare Industry in India and worldwide has undergone rapid transformations with effective and efficient digital delivery skills in recent years. It is expected to grow with each passing year. To positively manage the different spectrums of delivering excellence in wellness, healthcare management today is as vital as knowing the technical whereabouts of implementing best healthcare practices worldwide.
Therefore, the Healthcare Management in India must be equipped with learning interventions at regular intervals, facilitating the medical professionals with specific skill sets on a comprehensive and holistic understanding of strategic positioning, outreach, and communication through innovative programs and thought leadership.